Mental illness doesn’t discriminate. In fact, every year one-fifth of Americans experiences a clinical mental health disorder, whether or not they are diagnosed or receive treatment. That means that even if you haven’t personally experienced a mental health crisis, you certainly know someone who has, even if they don’t talk about it.
Unfortunately, despite the serious impact of mental illness on society – mental health disorders are, for example, a key reason for lost economic productivity – our existing mental health care system isn’t equipped to support patients and their families. There aren’t enough practitioners, especially outside of major cities, many don’t take insurance, and waiting lists can stretch on for months for top programs. That’s why a growing number of people are turning to the digital world for care, with IoT and other connected tech presented as the perfect way to bridge the care gap.
The Basics: Telehealth
When we think about healthcare innovations, we often leap to the extremes like robotic surgery and deep brain stimulation, but in its simplest form, digital mental health care is just online therapy. For a variety of reasons, conventional therapy isn’t accessible to many people, often because they have to work during typical practice hours or because they live in a rural part of the country without enough doctors; according to a recent Washington Post report on medical deserts, 20% of Americans live in rural areas, but these areas only have 10% of Americas doctors, and an even lower percentage of its specialists. Telehealth programs now serve as a key link to more advanced care, whether that means calling for a neurology consult after someone has a stroke or setting up weekly meetings with a therapist.
Until recently, security represented a major challenge for telehealth providers. In the last few years, though, a number of HIPAA-compliant telehealth programs have come to market. Depending on patient needs, telehealth providers can even employ biometric sensors to collect medical and lifestyle data to improve care. This makes it possible for therapists to provide remote biofeedback sessions or for psychiatrists to monitor drug side effects. These are the types of services that are especially underrepresented, and that can be hard to access – particularly at a reasonable price. Technology can democratize access, as it has with other types of care.
In addition to more advanced telehealth programs, many people are also turning to digital therapy platforms for short-term care. While these apps, many of which are text-based, are typically less comprehensive than traditional mental health treatment and don’t allow patients to select specific providers, they’re a valuable tool for patients who aren’t sure if they should pursue in-person therapy or who are searching for a therapist. Even in major cities like New York, it can take time to call therapists, confirm insurance, and screen for a suitable provider, during which time app-based therapy programs can provide support.
Tracking Patients With Serious Mental Illness
The majority of those living with a mental health issue have highly-treatable anxiety or depression. Given access to therapy and medication, sometimes even just for a few months or years, these patients can generally resume their normal lives with few problems. They understand the impact of their illness and how to manage it and want to feel better, but not all patients are so easy to treat.
A much smaller but more vulnerable segment of those with a mental illness have what experts term serious mental illness (SMI), typically categorized as conditions associated with psychosis and other extreme states. For these individuals, mental illness is much more likely to lead to unemployment and homelessness, addiction, and erratic behavior. Particularly among those with schizophrenia and related disorders, SMI can also lead to anosognosia or the inability to recognize that they are ill. These patients may resist treatment, particularly medication, despite feeling much better and being highly functional when taking medications – and this is where new technology can help.
While there’s much debate about mandated psychiatric treatment, a growing number of areas are employing assisted outpatient treatment (AOT), in which patients are mandated by courts to take medication and placed under appropriate oversight. To assist in this program, drug manufacturers recently began producing the antipsychotic drug Abilify with tracking technology triggered by ingestion. The small sensors allow doctors or family members to ensure that typically non-compliant patients continue taking their medication and can also help foster independence.
Wearable Wellness Options
Fitbit, Apple Watch, Jawbone – we love fitness trackers. Though there’s little evidence that these devices actually make people more active or otherwise lead to measurable improvements in health, they represent the democratization and acceptance of wearable health technologies. More advanced wearables, particularly those like Apple Watch, can also coordinate with critical implanted tech like continuous glucose monitors to make sure patients with diabetes are within safe blood sugar parameters. While it’s easy to measure heart rate or glucose with worn or implanted sensors, though, can such technology really offer any insights about mental health?
This is the answer that researchers are currently pursuing, with Apple’s Cognitive Kit leading the way. Via the Cognitive Kit, patients can share real time mood data with their doctors, providing a broader view of emotional patterns than is typically available during treatment sessions. The Cognitive Kit is also equipped with games that may enhance cognitive flexibility and indicate reaction issues. Doctors hope that, in addition to supporting mental health treatment, it may also serve as an intervention for patients with Alzheimer’s disease.
Diagnostic Algorithms
It’s not uncommon for patients seeking mental health care to go without a diagnosis for months, especially if they’re receiving counseling but not psychiatric treatment. Doctors like to take some time to evaluate patients’ needs and circumstances thoroughly before drawing any conclusions. That’s because extenuating situations, like a death in the family, can cause temporary depression or it may take a while before patients are ready to disclose trauma, leading to a PTSD diagnosis. But what is there was a better – and faster – way to get to a diagnosis and move treatment forward? Some doctors and researchers think that algorithms might hold the key.
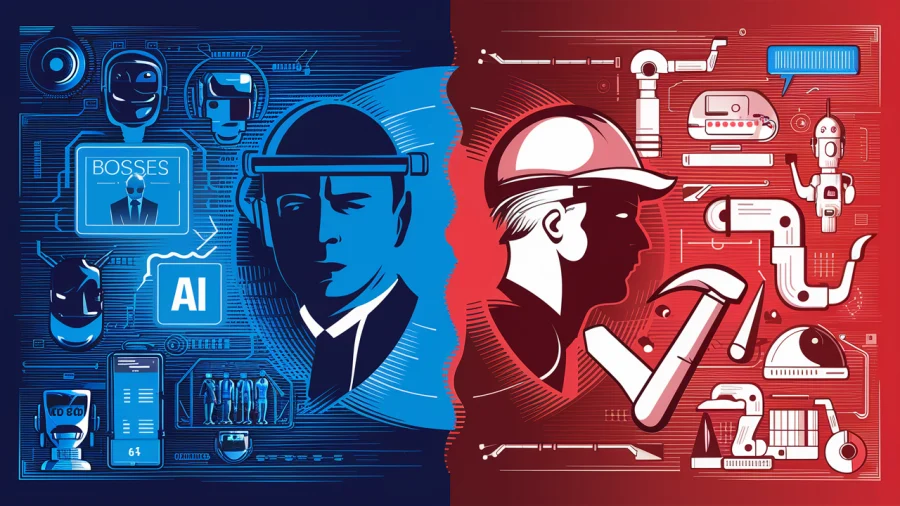
In a recent test using an AI algorithm on Facebook, researchers found the AI could detect signs of clinical depression three months before users’ medical providers diagnosed them, on average. The AI relies specifically on analysis of users’ posts, though it’s easy to imagine future, more advanced systems that could also monitor changes in the amount of social media use, searches and pages visited, and other indicators of mental distress.
On The Couch With The Computer
Despite major improvements overall, there’s still a great deal of stigma associated with seeking mental health care, especially among men and certain minority communities. If individuals could tell their problems to a computer, though, would they feel more comfortable with the process? A few mental health startups are testing this model, essentially by allowing users to examine their mood and thought patterns and then, based on this information, guiding them through cognitive behavioral therapy (CBT) skills.
Certain modes of treatment lend themselves better to the AI-based approach than others. Natural language processing is not yet at a point that it can handle complex conversation. However, many apps provide valuable skills-based strategies for managing anxiety and depression. If this can help people who would otherwise avoid all mental health care better manage their moods, that’s a step in the right direction.
Digital mental health care is still an emerging field, but there are already a number of powerful tools helping to reach patients who otherwise may not have access to care. Whether that means supporting those who struggle with medication compliance or offering off-hours, remote access to therapy via telemedicine, the growth in digital mental health reflects our changing social norms. We funnel all demands for service through digital platforms now, we wear tools that measure our vital statistics, and we trust the internet to support our healthcare decisions.
Mental health may be harder to measure in an objective sense, but that doesn’t mean we can’t use similar tools to improve our current model of care.