Netflix’s new “The Social Dilemma” documentary has been eye-opening for millions of viewers (see in: hundustantimes, dotcom), sparking conversation — and concern — about how the algorithms used by social media platforms manipulate human behavior.
Here is: “AI is Neutral Technology: What May be Harmful in Social Media Can Help Healthcare — By Dr. Darren Schulte, MD is Chief Executive Officer at Apixio.
By leveraging artificial intelligence that has become shockingly good at analyzing, predicting, and influencing user behavior. The film asserts that the resulting unintended consequences have created real-life dystopian implications: excessive screen time that causes real-world relationships to suffer, addictive behavior, alarming societal divisiveness, and even higher rates of depression, self-harm, and suicide.
These consequences as users look to social media for validation. Big tech corporations profit enormously by harvesting and analyzing their user data and manipulating their behavior to benefit advertisers.
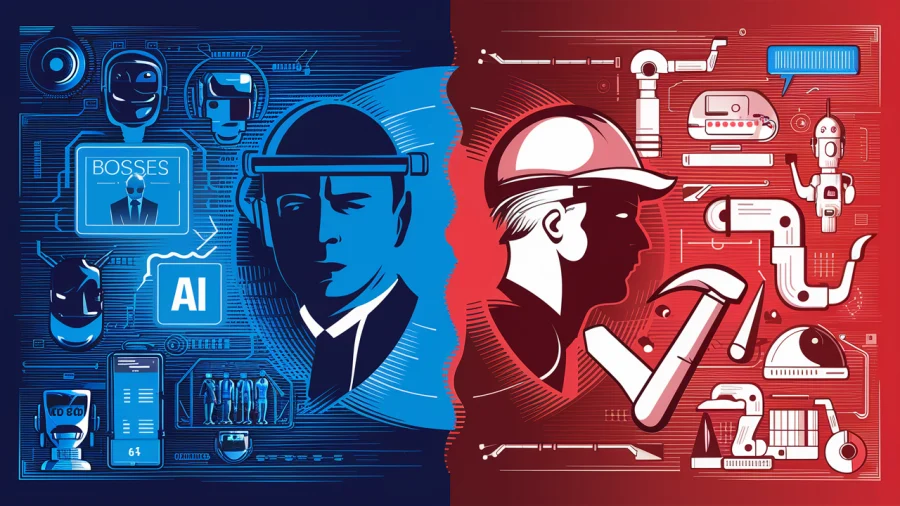
While the film appears to give machine learning algorithms a bad rap, these algorithms aren’t inherently evil. It all depends upon what the algorithms are trained to do.
In fact, the use of AI algorithms in healthcare has tremendous potential to transform health care by improving individual patient outcomes and overall population health, enabling more personalized medicine, reducing waste and costs, and accelerating the discovery of new treatment and preventative measures.
The same type of algorithms showcased in the Social Dilemma can be trained to analyze data generated by patients, care providers, and devices (like wearables).
The algorithms can even use surveillance of body functions (like lab tests and vital signs) to provide deeper and more accurate insight into individual health, health-related habits, and behaviors over time.
By combining that individual data with anonymous, aggregated population data, we can discover better treatments, refine clinical guidelines, and discover new therapies to improve overall population health.
Let’s consider these 11 ways AI can benefit health care applications.
- Improve response to emergent diseases like COVID-19. One of the problems we’ve had with effectively treating COVID-19 patients is that there’s been a lot of experimentation and trial-and-error. However, even the data on the results of those therapies has been slow to propagate across the global medical community.
Hospitals and physicians only have data on the patients that they are treating themselves. With no cohesive system for sharing patient data. Providers in America, for example, have not been able to benefit quickly enough from the knowledge and experience of providers in Asia and Europe — where the virus spread first.
By leveraging AI to mine aggregated medical records from millions of individuals, we could see what treatments have been most effective for specific patient cohorts.
Even further, we could analyze the characteristics of those already infected to see which attributes make one more likely to develop the most severe symptoms. By identifying vulnerable populations faster, we can then take targeted steps to prevent infection and implement the most effective treatments.
As we have seen, the analysis and exchange of this data manually, takes far too long, contributing to the propagation and death toll. With AI, we can surface this knowledge much faster and potentially reduce the impact of the next novel disease.
- Provide better patient surveillance. Identifying how – and how fast – COVID-19 spreads has also been a significant challenge. Scientists traditionally use a metric called R0 (pronounced “R naught”), a measure of the average number of people infected by one infectious individual.
Using R0 to predict COVID-19’s spread has been problematic for several reasons, including the fact that different groups use different models and data, and asymptomatic individuals can spread the disease without knowing that they are infected.
AI can help resolve this issue to improve patient surveillance by analyzing both medical records of patients who tested positive alongside contact tracing data that indicates the potential for infection. By combining this data and analyzing it at scale, medical authorities can use this insight to determine where to implement aggressive testing programs and more restrictive shelter-in-place measures to slow the spread of disease.
- Improve the quality of care. Health care providers want to deliver the best quality of care to their patients. But one of the challenges they face is measuring quality and patient outcomes with empirical evidence. With patient data scattered across different sources like electronic health records (EHRs), lab results, imaging studies, it is difficult to aggregate and analyze.
By implementing systems that consolidate this data and allow providers to use AI to mine it for insights, physician practices and hospitals can identify trends among patients and implement quality improvement programs.
For example, if they see that individuals with certain characteristics fail to follow-up on important health concerns, providers can intervene with appointment reminders, transportation resources, provide telehealth options, or other interventions to keep patients engaged in their own care.
On the flip side, insurers are also concerned about care quality and ensuring patients get the best possible outcome at the lowest possible cost.
AI can help insurers track and measure patient outcomes as they move through the care system—from a primary care provider to a specialist to a hospital for surgery and into a rehab facility, for example—and identify providers or treatment protocols that may not be delivering optimal results. Insurers can then work with providers to implement new approaches to improve success rates and overall patient outcomes.
- Identify and mitigate concerning trends. During a typical patient encounter, doctors only have access to the medical information for the patient in front of them. Consulting their patient history provides a limited view of factors that might indicate declining health. With data scattered across different systems, doctors do not always have all the data they need at hand.
AI can help surface broader indicators that a patient’s health may be declining over time.
By analyzing aggregate data across a large population, AI can show that patients with certain vital signs or trends in their data might be headed toward developing certain conditions, like diabetes or heart disease.
Physicians can use this information as a predictor of potential trouble and begin implementing preventative action. Some solutions can alert physicians to these insights as notifications within the Electronic Health Record (EHR) during the patient encounter. This allows physicians to take swift action to prevent disease progression.
- Enable personalized medicine. The health care industry has been moving toward personalized medicine for years, aiming to transform the “one-size-fits-all” approach to care into a customized plan for each individual. But this is practically impossible without access to aggregated data and insights that only AI can provide.
Consider the AI social media companies use to create and leverage personas to prompt engagement and drive advertising dollars. If we were to apply the same technique to build health care personas for each person, we could then provide this information to providers (with the patient’s permission).
Providers could then use tools like notifications, nudges, cues, or other communication (just like social media) to elicit positive behavior for better health.
For example, providers could target at-risk patients with prescription reminders, diet recommendations, or other resources relevant to their specific health situation.
- Reduce diagnostic and treatment errors. Even the best providers can overlook important details and make mistakes, especially with the pressure they are under to squeeze more patients into a typical day.
Just as algorithms can help social platforms surface insights about their audience to woo advertisers, physicians can use algorithms to surface insights to diagnose and treat conditions accurately. For example, AI can highlight confounding conditions or risk factors for patients, allowing doctors to consider the individual’s entire health profile when making decisions.
AI can also aid in surfacing potential drug interactions that could put patients at risk. All of this can substantially lower the risk of errors that cause patients harm, not to mention reduce the risk of malpractice accusations.
- Enable early intervention for high-risk patients. Just 5% of Americans account for 50% of all health care spending. These “high utilizers” often have chronic conditions that require constant care, which is why early diagnosis, intervention, and prevention are critical.
The same way algorithms can identify Facebook users who might be interested in a new lawnmower and serve up an appropriate ad; they can help providers identify high-risk patients before they develop costly care needs. By culling through data to identify risk factors, AI allows providers to implement preventative and early intervention strategies.
For example, an algorithm might spot a specific obesity indicator that correlates with the risk for Type II diabetes or identify patients with high blood pressure that are at greater risk of heart attack, stroke, or kidney disease.
These insights can be delivered at the point of care, even during a patient encounter. If a patient displays a specific set of symptoms, as the data is entered into the EHR, the physician is alerted to the risk and can review trends in disease progression or confounding conditions to plot the best course of action.
- Identify optimal treatment pathways through data-based referrals. Traditionally, when a patient needed to see a specialist, for surgery or physical therapy, for example, physicians typically referred to providers with whom they have existing relationships.
Unfortunately for patients, this does not always mean they get the best care for their unique situation. Does the provider have experience working with patients with co-morbidities? Do they specialize in complex surgeries or more typical procedures?
AI allows providers to refer to the best provider for each patient’s unique needs based on hard evidence of success and proven outcomes, rather than simply based on existing ties.
For example, if a patient with diabetes needs a knee replacement, AI can help primary care providers to identify orthopedic specialists and rehabilitation providers with proven, demonstrably better results in handling patients with this co-existing condition.
- Reduce spending waste. About 30% of healthcare spending is considered “waste,” totaling up to $935 billion. Nearly $80 billion alone can be attributed to overtreatment or low-value care.
In other words, providers order more tests, services, and procedures that aren’t necessarily the best option—or even necessary at all—mostly in an effort to protect themselves against being accused of not doing enough and to meet insurer’s requirements (e.g., ordering x-rays before an MRI when an injury is clearly soft tissue related or sending patients for multiple repeat mammograms before conducting an ultrasound to evaluate a suspicious lump).
By mining data using algorithms, providers and insurers can focus on using the tests and procedures that demonstrate high value or necessary for specific instances. For example, is it necessary for patients on certain medications to get blood tests every 90 days? Do wellness visits add value to patients?
By looking at what is most effective across the larger population, AI can help point physicians in the right direction earlier, reducing unnecessary diagnostics and placing the patient on the path to better health more quickly.
AI thereby can reduce wasteful spending by identifying diagnostics that are most effective and economical, potentially saving patients and payers millions every year on ineffective tests and treatments.
- Accelerate drug and treatment discovery. The current pathway to new drugs, vaccines, and treatments is long and arduous. On average, it takes at least ten years for new drugs to go from discovery to marketplace, with trials alone taking as long as seven years on average. For new vaccines, the average time to market is up to 12 years (which puts hope for a COVID-19 vaccine by year’s end into perspective).
One of the reasons the process is so slow is the lack of advanced data and analytics capabilities in the process.
The use of AI to analyze patient and drug performance data could substantially accelerate the time to market for new drugs and vaccines, which could save lives.
Just as the lack of data analytics meant doctors struggled to devise effective COVID-19 protocols, the inability to rapidly analyze trial data and evaluate new use cases for existing drugs prevents patients from getting the treatment they need.
Algorithms can accelerate this analysis and get much-needed medicines into the hands of patients faster.
- Lower operational costs. Doctors spend about one-sixth of their time on administrative work on average, with nearly a third of the doctors spending 20 hours or more each week on paperwork and admin tasks. And this does not include other operational tasks like coding, documentation, and reporting done by support staff.
All this time can add up to a significant cost and take away from time spent in direct, face-to-face time with patients.
AI can help reduce this burden and lower operational costs by automating manual processes like prior authorizations, reducing retrospective chart reviews by surfacing the right data to the right people earlier. The right data, quickly obtainable, will help physicians make better, faster decisions.
These efficiencies enabled by AI, on the administrative side, ultimately lower the cost of health care services for both patients and payers and frees up more resources to improve direct patient care.
The negative use of social media comes when the data influences human behavior bringing negative consequences.
For the most part, technology is neutral. But in the wrong hands with the wrong motives or objectives, the use of algorithms can raise serious ethical questions.
The same algorithms that cause us to feel more anxious, isolated, or depressed when leveraged by social media can also be used to help us heal, stay healthy, and achieve optimal well-being.
The questions are all about the algorithm’s objective and training, testing, and user feedback data that are used by the algorithm. The reality is that managing both individual and public health in the 21st century requires access to data and insights.
Without data-driven insights, we are just guessing what will work in healthcare and what doesn’t.
Leveraging algorithms to analyze health care data empowers physicians to devise a truly personalized care plan for each individual. The physician can improve the quality of care overall and lower health care costs by tapping into collective insight and knowledge gleaned from millions of patient records.
Image Credit: karolina grabowska; pexels